A recent study posted to the medRxiv* preprint server evaluated whether SCENtinel 1.1 could rapidly screen for coronavirus disease 2019 (COVID-19)-associated olfactory abnormalities.
Background
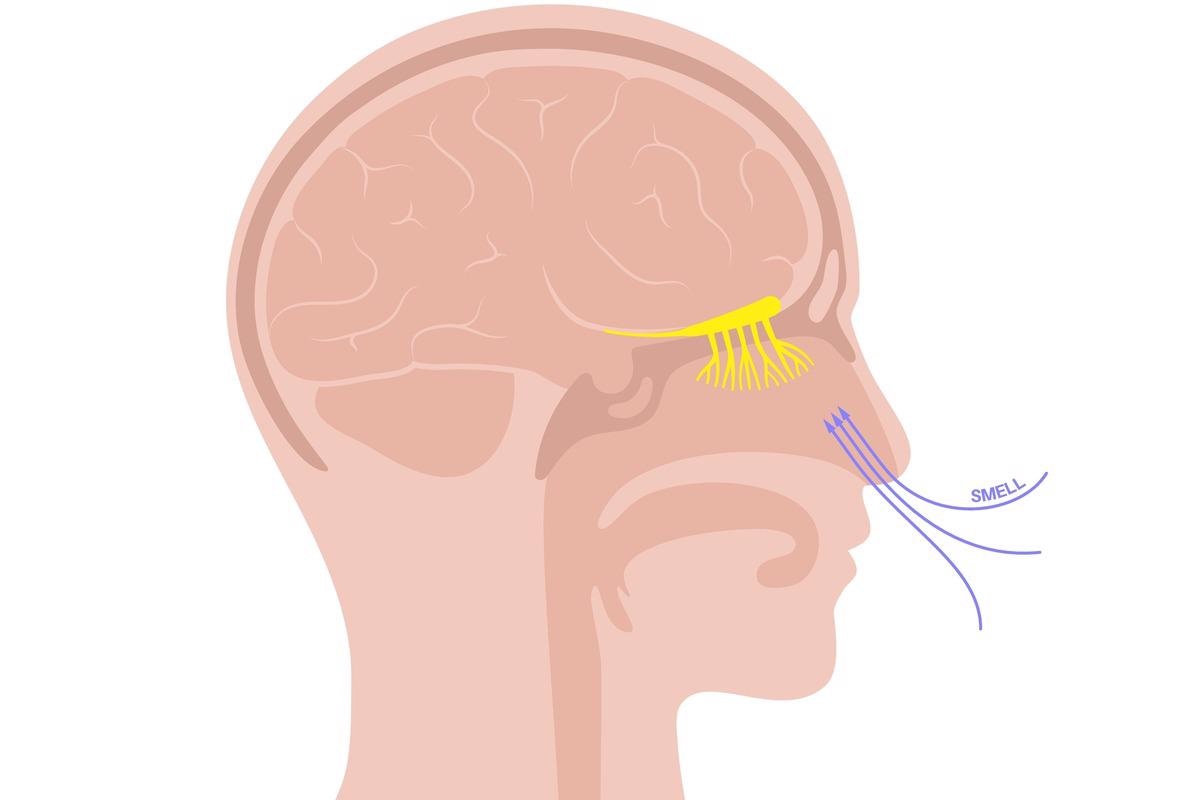
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic increased the incidence of people experiencing olfactory disorders. Nearly half of the individuals infected with COVID-19 reported a loss of their odor sensing capacity.
While most people regain their sense of smell in three weeks, approximately 10-15% suffer persistent anosmia that lasts longer than a month in duration. However, population-wide and rapid olfactory testing have been scarce during the COVID-19 pandemic.
The present study's authors had previously created a rapid and economic modality, SCENTinel 1.0, for evaluating odor detection, odor identification capacity, and odor intensity in SARS-CoV-2-infected individuals. SCENTinel 1.0 could distinguish between normosmia (normal sense of smell) and anosmia (total loss of smell) from a single odor.
About the study
In the present work, the scientists established a novel version of SCENTinel 1.0, known as SCENTinel 1.1, adding a hedonic subtest (how pleasant is the odor) and one of the four potential smells to the original mix. The four new target odors were bubblegum, flowers, caramel popcorn, and coffee. These new targets allowed multiple assessments of 12 distinct odor pairings and provided a collection of odor-specific olfactory symptoms.
The goal of this investigation was to 1) validate SCENTinel 1.1 in various cohorts of subjects with anosmia and normosmia employing SCENTinel 1.0's original model, 2) identify if SCENTinel 1.1 could distinguish between the quantitative and qualitative olfactory abnormalities that were frequent in SARS-CoV-2 infections, and 3) use the capacity of hedonic score to detect parosmia.
Subjects were enrolled via two Facebook groups: 1) AbScent Parosmia and Phantosmia Support, and 2) COVID-19 Smell and Taste Loss. This research included those aged 18 to 75 years residing in the United States and have access to a computer or smart device.
A total of 381 subjects were stratified into four categories according to their self-documented olfactory performance. The four groups were: 1) normosmia with 66 participants, 2) qualitative smell disorder, i.e., 86 subjects with phantosmia or parosmia, 3) quantitative smell disorder, i.e., 135 individuals with hyposmia or anosmia, and 4) 94 people who had both qualitative and quantitative olfactory complaints (mixed).
Findings
The results indicated that the revised SCENTinel version, SCENTinel 1.1, classified normosmia and anosmia with greater sensitivity, comparable to the SCENTinel 1.0. No variation in average intensity ratings or total scores were discovered between the four target scents employed in the SCENTinel 1.1. These coherent results in SCENTinel 1.1 and SCENTinel 1.0 across diverse research groups demonstrate that SCENTinel 1.1's enhancements, such as additional target scents, still efficiently monitor normosmia and anosmia.
SCENTinel 1.1 could also precisely distinguish between 1) quantitative and qualitative groups, 2) quantitative and normosmia, and 3) normosmia and qualitative groups. The SCENTinel 1.1 subtest found that the best-distinguished normosmia, quantitative, and qualitative groups varied based on group comparison.
Only the odor intensity subtest distinguished the qualitative and quantitative groups more than chance, with 88% of the qualitative group rating the odor intensity >20 compared to the quantitative group. The odor intensity and odor identification subtests were used to distinguish between the quantitative and normosmia groups. Further, the odor identification, hedonic score, and odor detection subsets distinguished qualitative and normosmia groups.
As predicted, 86% of people with normosmia satisfied the SCENTinel 1.1 overall score accuracy criterion, compared to 61% in the quantitative and 59% in the qualitative groups. In addition, the odor intensity ratings were higher in the normosmia and qualitative groups than in the quantitative group.
On the SCENTinel 1.1 test, 83% of the normosmia and 76% of the quantitative groups could accurately identify the odor compared to 63% in the qualitative group. Nevertheless, the percentage of participants in the qualitative and quantitative groups who satisfied the accuracy criterion for the SCENTinel 1.1 odor identification subtest did not differ substantially.
SCENTinel 1.1 distinguished between 1) hyposmia and anosmia, 2) hyposmia and parosmia, and 3) parosmia and anosmia more accurately than SCENTinel 1.0. Hedonic scores successfully identified people with parosmia. The hyposmia subjects' hedonic scores were superior to the parosmia patients. Moreover, the hedonic scores of subjects with parosmia were considerably lower than those in whom parosmia was absent, showing that the olfactory distortions were unpleasant in the initial set of patients.
Conclusions
The study findings demonstrated that SCENTinel 1.1 was a fast odor diagnostic that could distinguish between normosmia, quantitative (hyposmia, anosmia), and qualitative (phantosmia, parosmia) olfactory abnormalities. It was one of the few direct tests that could detect parosmia rapidly by evaluating hedonics. SCENTinel might be a valuable tool for assessing scent function in a variety of research and clinical situations.
The present study partially supports the use of hedonic scores to detect parosmia. However, more ongoing studies are needed to categorize olfactory diseases based on the SCENTinel criteria, and render them relevant in clinical or research settings. In addition, further studies are required to account for the influence of various etiologies of olfactory abnormalities (i.e., other than COVID-19).
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Stephanie R. Hunter, Mackenzie E. Hannum, Robert Pellegrino, Maureen A. O’Leary, Nancy E. Rawson, Danielle R. Reed, Pamela H. Dalton, Valentina Parma. (2022). SCENTinel 1.1 rapidly screens for COVID-19 related olfactory disorders. medRxiv. doi: https://doi.org/10.1101/2022.03.23.22272807 https://www.medrxiv.org/content/10.1101/2022.03.23.22272807v1
Posted in: Medical Science News | Disease/Infection News | Healthcare News
Tags: Anosmia, Coffee, Coronavirus, Coronavirus Disease COVID-19, covid-19, Diagnostic, Pandemic, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome

Written by
Shanet Susan Alex
Shanet Susan Alex, a medical writer, based in Kerala, India, is a Doctor of Pharmacy graduate from Kerala University of Health Sciences. Her academic background is in clinical pharmacy and research, and she is passionate about medical writing. Shanet has published papers in the International Journal of Medical Science and Current Research (IJMSCR), the International Journal of Pharmacy (IJP), and the International Journal of Medical Science and Applied Research (IJMSAR). Apart from work, she enjoys listening to music and watching movies.
Source: Read Full Article