With over 108 million reported infections from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) worldwide, and nearly 2.4 million deaths, the ongoing pandemic has jeopardized the physical, financial and emotional wellbeing of the global population over the past year. A new preprint research paper posted to the bioRxiv* server discusses the emergence of mutations in the SARS-CoV-2 virus, allowing it to escape the effects of the most commonly used antiviral drug, remdesivir.
In an effort to arrest the spread of SARS-CoV-2 infection, drug development and repurposing research has been proceeding at a rapid pace in multiple centers.
Remdesivir shows conflicting results
Among the few drugs that have been approved for the specific treatment of COVID-19 disease, remdesivir (RDV) has been extensively used. This drug is a broad-spectrum nucleoside analog, and its in vitro viral inhibitory activity has been impressive. In three randomized trials, its use was associated with accelerated recovery, with the time being reduced by a third. No significant benefits on mortality were observed
However, these findings contradicted a larger Solidarity Therapeutics Trial carried out by the World Health Organization (WHO), which demonstrated a lack of association between RDV and survival. The time of initiation of RDV is also, apparently, crucial to its action.
Nonetheless, many countries continue to use RDV as a first-line treatment for COVID-19 patients hospitalized with a need for oxygen supplementation within ten days of infection. Remdesivir is often used along with the anti-inflammatory glucocorticoid dexamethasone.
Mutations are a well-known viral mechanism to escape drug inhibition, especially during monotherapy. However, current literature does not contain any examples of RDV-resistant SARS-CoV-2 strains in circulation. The current study aims to understand whether such resistance can emerge and which mutations are responsible.
Study details
The researchers found that of 12 viral lineages passaged in media containing RDV at either 1 µM or 2.5 µM, seven showed cytopathic effects (CPE), indicating the virus's active replication the cell. The virus titer also increased by 0.5 to 1 log, indicating the virus was adapting to the Vero cells.
In two of the passaged virus lineages, the speed and magnitude of replication showed a change, as well as the concentration of RDV required to achieve 50% inhibition. These lineages actively replicated in the presence of 7.5 µM RDV. The titers were lower than when it was grown without RDV, however.
In Vero cells, these actively replicating strains showed a twofold increase in IC50, and a nearly fourfold increase relative to the parental strain. When the same viruses were passaged in media not containing RDV, the IC50 remained comparable with the parental strain.
This partial resistance to RDV was not replicated with other nucleoside analogs such as EIDD2801, indicating the emergence of specific resistance mutations.
E802 mutation
The researchers found two fixed non-synonymous mutations in these lineages, both of which were absent when the same strains were passaged in the absence of RD. These mutations were also not present in the original input virus or the ancestral Wuhan strain.
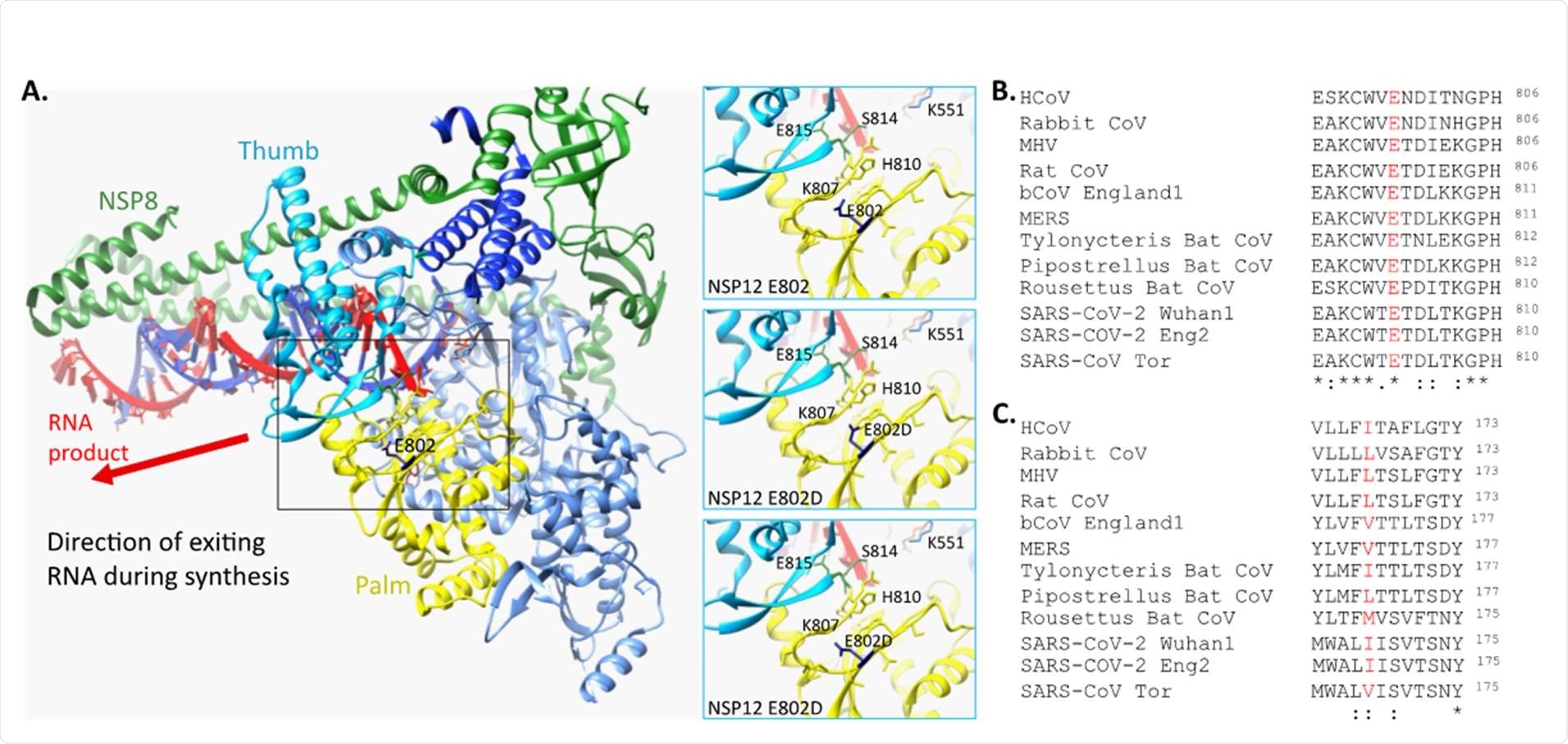
The first mutation was a glutamine to aspartate mutation (Glu802Asp; E802D) in the viral RNA-dependent RNA polymerase (RdRp) NSP12, similar to that observed in other betacoronaviruses that show reduced RDV sensitivity. It is noteworthy that glutamate at this position is found in all betacoronaviruses.
The E802 mutation occurs near amino acid residues that are predicted to form bonds with newly formed RNA. The researchers suggest that this results in small structural modifications that reduce steric hindrance in this region. The result is resistance to the inhibitory effects of RDV incorporation into the growing RNA molecule.
I168T mutation
The second mutation is a substitution of threonine for isoleucine (Ile168Thr; I168T) in NSP6. This highly conserved protein is found to limit the expansion of the autophagosome. The presence of this mutation could lead to a change in the structure of the transmembrane and extracellular domains of the protein.
These mutations are not found to affect viral fitness or peak viral titers. Either the E802D or E802A mutation was found to confer partial resistance to RDV, similar to that found in viral lineages serially passaged in RDV-supplemented media.
E802 substitutions raise IC50
With the E802D and E802A mutations in NSP12, the IC50 rose by twofold, and by 2.5-fold, respectively, irrespective of the type of cell used. Thus, the researchers rule out different cell-dependent metabolism pathways, or variations in virus entry or replication dependent on the viral lineage, as explanations for the emergence of these mutations.
Interestingly, viruses with both mutations had increased sensitivity to the drug relative to lineages with only the NSP12 mutation.
Secondly, either of the mutations was consistent with intact sensitivity to EIDD2801. Thirdly, when cultured in human airway-derived Calu-3 cells, the researchers found that the titer for all virus lineages was reduced, in correlation with the dose of RDV used.
However, the titers of viruses containing the NSP12-E802 mutation were higher at both 24 and 48 hours compared to the wildtype or NSP6-mutant viruses.
RDV-resistance mutations found in circulating strains
The study found eight viral genomic sequences with the E802 mutation, four with E802A and four with E802D. Seven of these were from RDV-treated patients, but one was not, suggesting selection for this mutation can occur without exposure to the drug. There were 33 sequences showing substitution of isoleucine at 1168 with other residues.
Globally, the E802 substitution is as common as other NSP12 mutations associated with partial resistance to RDV in other coronaviruses. Though rare, these mutations are demonstrated to be viable and can emerge as part of a resistant variant under selective pressure.
Compared with the input virus, the passaged viruses were more sensitive to RDV when grown in Vero cells in the absence of RDV than in its presence.
When compared to the input sequence, there were 41 non-synonymous and 10 synonymous mutations, but none in the proofreading NSP14 that would contribute to the altered sensitivity of the virus to RDV. The effect of RDV concentrations on the rate of viral mutation is thus unclear at present.
Most mutations affected the spike open reading frame, but not the furin-like cleavage site. Many of these mutations have been found in the emerging UK and South African variants. Only one, P681P, was present in the parental strain. The E484 mutation appeared in 20% to 40% of the virus lineages except one.
What are the implications?
Surprisingly, these mutations occurred in vitro, without any immune selection pressure.
"These observations underline the plasticity of the SARS-CoV-2 genome and also suggest that the independent emergence of different geographical variants sharing common mutations has not occurred due to selection pressure based on pre-existing immunity in the infected individuals."
Of 10 mutations in the passaged strains that were present in the input virus, five were found in over half of the population, and four became fixed by passage 13.
Overall, the study showed the emergence of a genome signature that confers partial resistance to RDV in the presence of the drug in vitro. This demonstrates the possibility of selection for RDV resistance. However, considering the extensive use of this drug, the rarity of the mutation rules out the global spread of such resistant variants.
The findings also show the occurrence of the key mutations that are characteristically found in the newer variants of concern in vitro, without exposure to human immune antibodies.
"Our study offers new perspectives for the surveillance of new SARS-CoV-2 variants and the clinical management of patients treated with RDV."
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Szemiel, A. M. et al. (2021). In vitro evolution of Remdesivir resistance reveals genome plasticity of SARS-CoV-2. bioRxiv preprint. doi: https://doi.org/10.1101/2021.02.01.429199. https://www.biorxiv.org/content/10.1101/2021.02.01.429199v1
Posted in: Medical Research News | Disease/Infection News
Tags: Amino Acid, Antibodies, Anti-Inflammatory, Antiviral Drug, Cell, Coronavirus, Coronavirus Disease COVID-19, Dexamethasone, Drugs, Genome, Genomic, Glucocorticoid, Glutamine, in vitro, Isoleucine, Metabolism, Molecule, Mortality, Mutation, Nucleoside, Oxygen, Pandemic, Polymerase, Protein, Remdesivir, Research, Respiratory, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Therapeutics, Threonine, Virus

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article
