A recent study published in the Indian Journal of Critical Care Medicine presented a case series of patients with coronavirus disease 2019 (COVID-19)-associated pulmonary aspergillosis (CAPA). The goal of the study was to inform clinicians and healthcare workers of this serious COVID-19-related complication.
Background
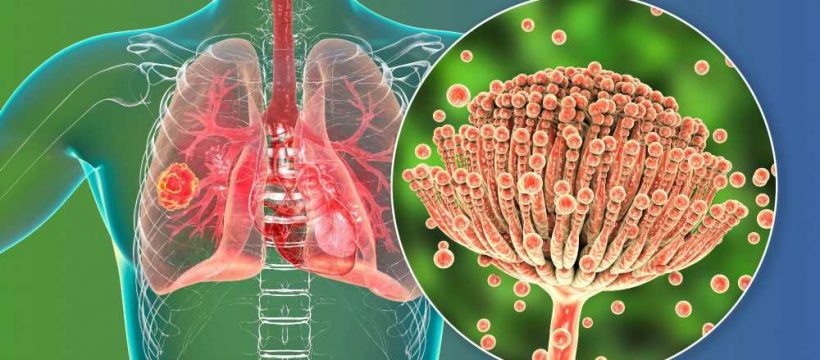
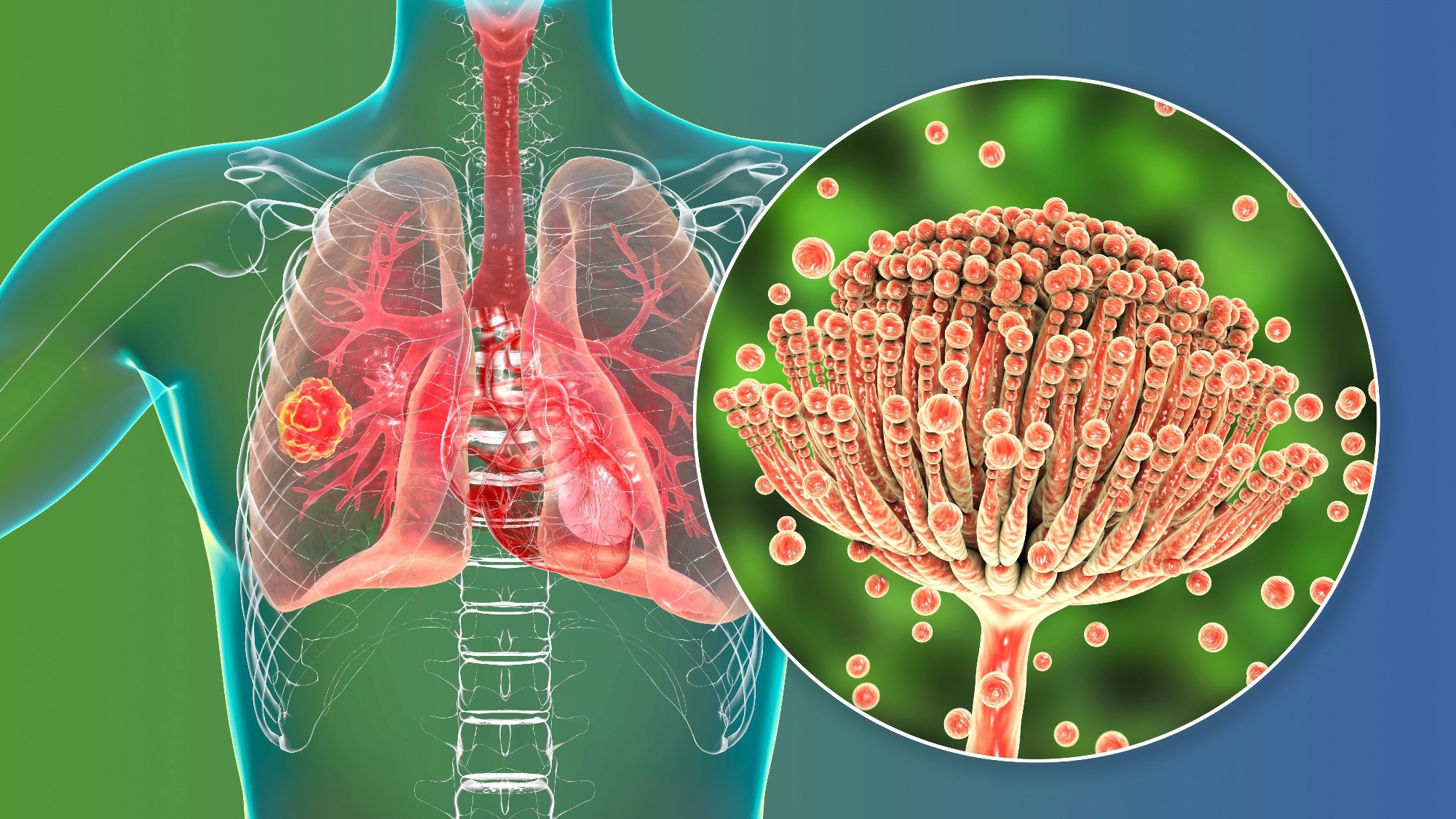
Many atypical radiological signs of COVID-19 and invasive pulmonary aspergillosis (IPA) mimic each other. Although IPA is most common in immunocompromised patients, influenza infection also increases its risk in non-neutropenic patients. Respiratory viruses damage the respiratory epithelium and paralyze the local immune system. This damage leads to secondary and opportunistic infections, including invasive fungal infections.
Thus, critically ill COVID-19 patients with acute respiratory distress syndrome (ARDS) admitted to intensive care units (ICUs) are prone to developing CAPA. Keeping this in mind and the occurrence of influenza-associated aspergillosis (IAA), IPA diagnosis is a must for COVID-19 patients as well. However, it is worth noting that radiology alone cannot always accurately diagnose CAPA in COVID-19 patients.
About the study
In the present study, researchers retrospectively reviewed the medical charts of all the COVID-19 patients who visited the Orchid Medical Centre in Ranchi, India. These patients had reverse transcription-polymerase chain reaction (RT-PCR)-confirmed COVID-19. First, the doctors prescribed supportive home treatment. However, when the patient's symptoms worsened, they advised hospital admission for further diagnosis and treatment.
Study findings
High-resolution computed tomography (HRCT) showed cavitary lesions in the lungs of these patients. Although HRCT findings pointed to the possibility of CAPA, they also performed a serum galactomannan test to enhance the diagnosis. Serum galactomannan assay was positive for all the patients. Due to the risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission and aerosolization, doctors avoided bronchoscopy. Instead, they prescribed an antifungal drug, voriconazole, at a dosage of 6 mg/kg every 12 hours intravenously for the first two days, followed by 4 mg/kg every 12 hours (maintenance dose).
Other ICU patients did not develop IPA, and even these patients were not immunocompromised. In the absence of any other factor that made these patients prone to this infection, severe COVID-19 emerged as the sole reason for developing IPA.
Conclusions
To summarize, it is difficult to differentiate between fungal colonization and invasive disease without bronchoscopic sampling and microscopic evaluation of fungal cultures. Antigen-based laboratory test galactomannan assay supports IPA diagnosis, but a more thorough approach is needed to define and diagnose IPA in COVID-19 patients. For instance, tissue culture and tissue microscopy of primarily sterile specimens showing invasive growth of septate fungal hyphae could confirm IPA diagnosis. Further, despite the risk posed by biopsies in COVID-19 patients, bronchoalveolar lavage fluid and lung biopsy are the best sample types to confirm IPA diagnosis in COVID-19 patients.
The present case series indicated an increased risk of developing IPA in critically ill COVID-19 patients, delayed diagnosis of which could translate into increased mortality and unnecessary burden on healthcare systems. Thus, clinicians should always look for CAPA in critically ill COVID-19 patients who are unresponsive to the treatment.
- Khushboo Sharma, Rash Kujur, Saurabh Sharma, Nishith Kumar, Manoj Kumar Ray. (2022). COVID-19-associated Pulmonary Aspergillosis: A Case Series. The Indian Journal of Critical Care Medicine. https://www.ncbi.nlm.nih.gov/research/coronavirus/publication/36213710
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Acute Respiratory Distress Syndrome, Antifungal, Antigen, Aspergillosis, Assay, Biopsy, Bronchoscopy, Computed Tomography, Coronavirus, Coronavirus Disease COVID-19, covid-19, Critical Care, Healthcare, Hospital, Immune System, Influenza, Intensive Care, Laboratory, Lungs, Medicine, Microscopy, Mortality, Polymerase, Polymerase Chain Reaction, Radiology, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Tissue Culture, Tomography, Transcription, Voriconazole

Written by
Neha Mathur
Neha is a digital marketing professional based in Gurugram, India. She has a Master’s degree from the University of Rajasthan with a specialization in Biotechnology in 2008. She has experience in pre-clinical research as part of her research project in The Department of Toxicology at the prestigious Central Drug Research Institute (CDRI), Lucknow, India. She also holds a certification in C++ programming.
Source: Read Full Article