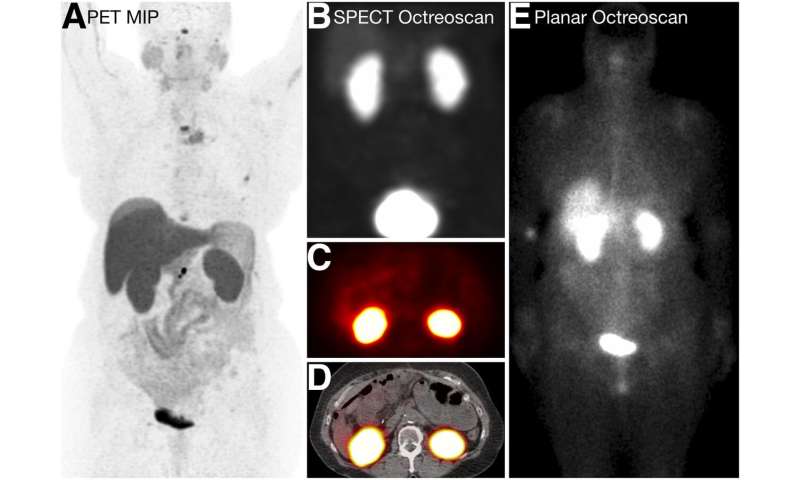
A new study published in The Journal of Nuclear Medicine evaluated the role of 68Ga-DOTATATE positron emission tomography/computed tomography (PET/CT) in selecting neuroendocrine tumor patients who may benefit from peptide receptor radionuclide therapy (PRRT). Although historically guided by a Krenning score based on 111In-pentetreotide scintigraphy, researchers found that Krenning scores based on PET/CT imaging were significantly higher and could more accurately detect patients eligible for PRRT. This is particularly relevant for patients with lesions of less than two centimeters, as the study showed that Krenning scores for these small-volume tumors were markedly higher when informed by PET/CT compared to 111In-pentetreotide scintigraphy and could qualify the patients for PRRT when they would otherwise have been ineligible.
“In the past, physicians relied on 111In-pentetreotide imaging with planar scintigraphy and single photon emission computed tomography (SPECT) to determine whether or not a patient is eligible to receive 177Lu-DOTATATE PRRT,” said Thomas A. Hope, MD, associate professor of radiology at the University of California, San Francisco. “However, limited literature is available on the accuracy of PET/CT in determining 177Lu-DOTATATE PRRT eligibility. Our study aimed to compare the Krenning scores derived from the various imaging modalities and assess the impact on treatment decision-making.”
The Krenning score is a relatively simple and reproducible method based on nuclear imaging used by physicians to make a quantitative estimate of the expression of somatostatin receptors (SSTR) in patients with neuroendocrine tumors. “Nuclear medicine physicians grade visually the uptake of the radiopharmaceutical in target lesions as compared to the uptake in the liver. This visual assessment is based on the target lesion with the highest uptake,” said Jeremie Calais, MD, assistant professor of nuclear medicine and theranostics at the University of California, Los Angeles. Hope added, “The higher the Krenning score, the higher the predicted uptake of the targeted therapy.”
The retrospective study included 150 patients with suspicion of or biochemical evidence of neuroendocrine tumors. Patients underwent both 68Ga-DOTATATE PET/CT and 111In-pentetreotide imaging (planar scintigraphy and SPECT) within a span of less than one week. Three physician readers independently analyzed all imaging studies and graded them using the Krenning score based on the lesion with the highest uptake. The studies were reviewed after grading, and a consensus grade was created for each study. The volume and extent of tumor burden, lesion size and maximum standardized uptake value also were measured and compared with the Krenning scores.
Based on the Krenning score, the detection rate of SSTR-positive disease was 23 percent, 38 percent and 72 percent with 111In-pentetreotide planar imaging, SPECT and 68Ga-DOTATATE PET/CT, respectively. The Krenning score was significantly higher with 68Ga-DOTATATE PET/CT than with the other modalities. Additionally, in patients with a Krenning score of at least three, the detection rate of 111In-pentetreotide planar imaging and SPECT was much lower with lesions smaller than two centimeters (15 and 24 percent) than with lesions larger than two centimeters (78 and 89 percent).
“This head-to-head comparison research study shows for the first time that 68Ga-DOTATATE PET/CT results in higher Krenning scores than 111In-pentetreotide imaging in determining eligibility for PRRT, especially for neuroendocrine tumor patients with lesions smaller than two centimeters,” Calais said. Most patients with lesions less than two centimeters would not have qualified for PRRT based on 111In-pentetreotide imaging but would appear to be candidates based on 68Ga-DOTATATE PET/CT.
“This is of significant importance as the NETTER-1 trial—the international phase 3 clinical trial that proved the effectiveness of 177Lu-DOTATATE PRRT and led to the approval of 177Lu-DOTATATE PRRT—included only patients screened with 111In-pentetreotide imaging,” said Calais. “The results of the NETTER-1 trial should not be directly applied to patients with smaller lesions, as small lesions are typically negative on 111In-pentetreotide scintigraphy and were not included in the trial. Many people assume the results of the NETTER-1 trial can be directly translated to patients screened with 68Ga-DOTATATE PET/CT—which could be true but has never been formally proven.”
Source: Read Full Article
