Patients who undergo skin injuries endure hospital stays, infection and/or succumb to death; therefore, advances in wound healing aim to improve clinical practices underlying macroscale healing to effectively intervene in microscale pathophysiology. As a result, strategies that optimize wound healing have motivated the design of new therapeutic products.
In a new report in Science Advances, Benjamin Freedman and a team of researchers in the School of Engineering, the Wyss Institute for Biologically Inspired Engineering, and the Brigham Women’s Hospital, Harvard, summarized advances in the development of new drugs, biomaterial therapies and biological products suited for wound healing. They classified the products as marketed therapies and agents for clinical trials to explore their successful and accelerated translation for wound healing.
The dynamics of chronic wound healing mechanisms
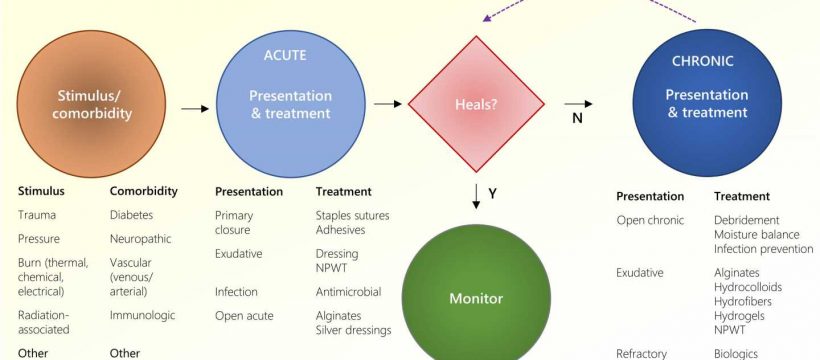
The timeframe of wound healing can vary and affect the process of patient recovery. Most wounds are classified as acute or chronic situations according to their clinical presentations. Untreated wounds can undergo cell death and necrosis, and represent ischemia relative to inadequate circulation due to microvascular damage and vasoconstriction. The nutritional status, fibroblast cell and progenitor health, as well as infectious bioburden, can contribute to disease progression.
Normal healing is associated with a series of events, including inflammation, remodeling and repair. Wounds that do not proceed through normal phases remain in a dysregulated inflammatory state with several delineating nuances.
For example, pressure ulcers result from an increasing depth of tissue necrosis and pain from microvascular injury causing ulceration and skin degradation to reach underlying fat or deeper structures. The resulting wounds require specialty care. Bioengineers and materials scientists in medical research have formed extensive libraries of wound care technologies to facilitate progressive healing.
The economic cost of wound care
Freedman and colleagues observed the economic challenges of wound care on health care systems that showed an increasing risk in patients with age and obesity alongside those who presented with high-risk comorbidities. Surgical wounds are the largest wound subset, accounting for careful surgical techniques and optimal suture materials in hospitals. Existing standards for interventional healing rely on the preparation of a viable wound bed for assisted healing to remove foreign materials and ischemic tissue. More complex wounds require secondary healing or a bridge for closure. Pressure injuries represent a more serious problem in bedridden patients.

The team listed the principles of open wound management as follows:
- Moisture balance
- Infection prevention
- Medical optimization of comorbidities including vascular disease and blood glucose control
They discussed the possibilities of minimizing inflammation, and progression towards active proliferation as a healing response. Several methods in the market aim to detect elevated protease activity for impaired wounds, and apply topical oxygen therapy and ultrasound therapy.
Newer and better interventional healing
The study outcomes highlighted the need for additional strategies, including healing the chronic wounds at complex and intricate levels. Most advances in intervention target coordinated cellular processes to optimize wound care, however, such methods remain incompletely understood, requiring ongoing research innovations. Freedman and the team described the primary aim of existing commercially available interventional biomaterials to impart fluid exudation, moisture balance, and pressure relief to prevent infection.
The advanced biomaterials in development for interventional healing can mimic extracellular matrix-inspired biophysical cues to regulate immune responses to treat and resolve inflammation. Such advances can be delivered to treat patients at the cellular level, where hydrogel influenced delivery systems can allow the sustained release of stimuli-responsive drug molecules to assist patients in adhering to new therapies. The outcomes can facilitate clinical trials of new drugs and biological products to therapeutically interfere in acute and chronic wounds.
Preclinical and clinical advances in wound healing
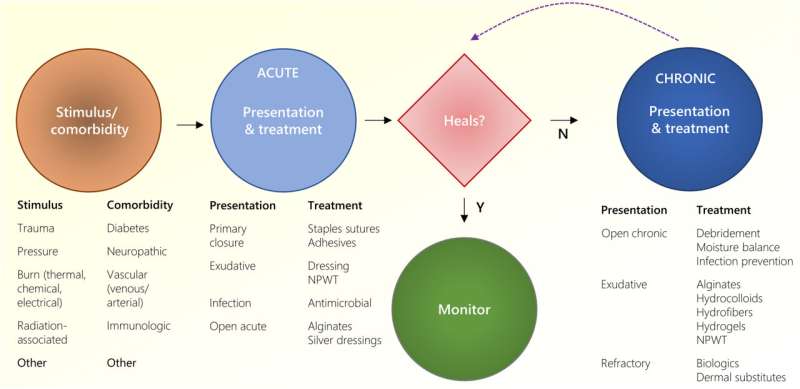
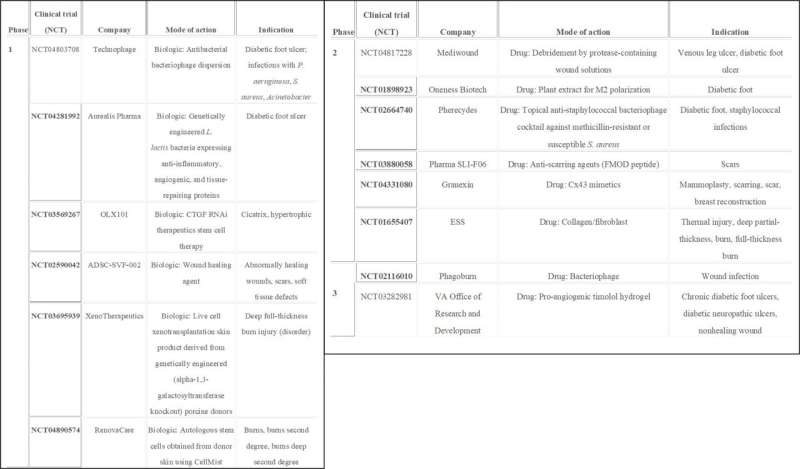
Acute wounds arising from surgical and traumatic events can be treated with bandages to inhibit bleeding and effectively promote healing. Researchers have recently combined adhesive hydrogels with surgical meshes to demonstrate their strong adhesion and flexibility under mechanical stress. Freedman and colleagues described existing advanced wound therapies in the clinical pipeline for wound management, anti-infection and biological intervention. These include advanced anti-scarring and healing-promoting therapies. For example, a cell-penetrating asymmetric interfering RNA delivered as an intradermal injection can target connective tissue growth factor to combat scarring.
New peptide formulas engineered to treat venous leg ulcers and diabetic foot ulcers are currently in phase 1 and 2 clinical trials. Next-generation therapies to treat burns are also in clinical trials. For instance, commercially available NexoBrid is a topical agent made of enzymes isolated from a pineapple plant containing a few proteinases to provide selective and quick removal of damaged/dead tissues within hours of application. Phase 3 clinical trial outcomes have shown the impact of the topical agent on healing tissue areas of interest without adverse serious effects. Several cell-based therapies are also similarly under study for adequate intervention.
Outlook: Innovative wound healing
In this way, Benjamin Freedman and colleagues summarized multiple methods of interventional wound care and detailed their mechanisms-of-action in preclinical and clinical environments to treat acute and chronic wounds. These methods focus on highly diverse phases of wound healing, including tight closure of the wound to establish homeostasis and modulate the immune system during inflammation, and cell proliferation alongside remodeling in the area of intervention. The bioengineers and materials scientists hope that future wound dressings may sense the unique environment of an inflicted region to deliver personalized strategies to autonomously regulate drug doses for every patient.
As a strategic plan-of-work for bioengineers, Freedman and the team suggest developing an evidence-based target profile and patenting strategy to effectively translate new wound care products from the bench to the bedside in health care. The industrial translation of standard care requires strong clinical data for emerging methods to survive beyond the bench and positively influence the quality of life of patients.
More information:
Benjamin R. Freedman et al, Breakthrough treatments for accelerated wound healing, Science Advances (2023). DOI: 10.1126/sciadv.ade7007
Journal information:
Science Advances
Source: Read Full Article