An international team led by investigators at McLean Hospital has analyzed the genes expressed in approximately 575,000 individual cells from the brains of people with and without post-traumatic stress and major depressive disorders (PTSD and MDD), revealing new insights into the mechanisms behind the brain’s stress response in these conditions.
The findings, which are published in The American Journal of Psychiatry, could lead to novel markers of PTSD and MDD and well as new therapeutic targets.
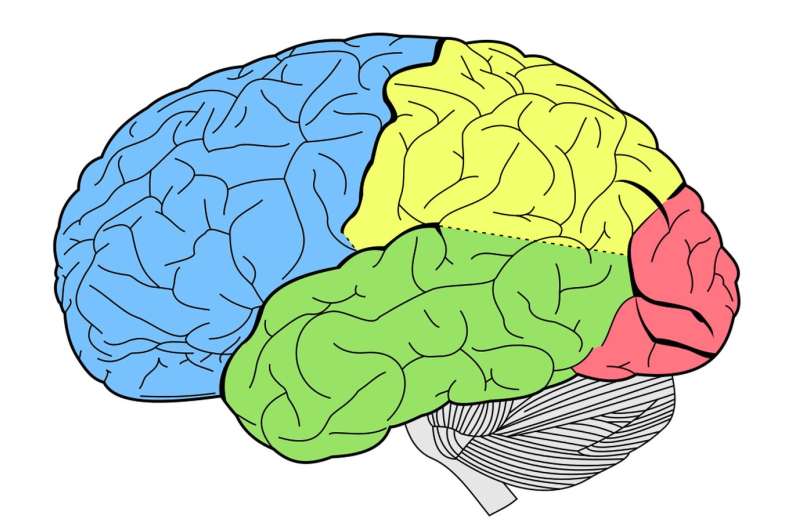
Because studies have implicated the dorsolateral prefrontal cortex (DLPFC) region of the brain in PTSD and MDD, the scientists compared the genes expressed in cells in DLPFC samples collected postmortem from 11 individuals with PTSD, 10 with MDD, and 11 without either of these conditions with a replication dataset half the size. The researchers detected which genes were expressed by which cells—including eight different types of cells—through a technique called single-cell RNA sequencing.
The analysis indicated that certain genes are expressed at varying levels in DLPFC neurons and astrocytes (a type of cell that supports neurons) depending on whether an individual had PTSD, MDD, or neither condition. For example, differential gene expression indicated increased glucocorticoid signaling in the brains of people with PTSD.
Various other pathways also had differential expression of genes across the study groups, suggesting that these pathways may be dysregulated in MDD or PTSD. Some of the genes that were identified were located in a region of chromosome 17 that has been implicated in neurodevelopmental and neurodegenerative disorders.
“Our findings can be used in the development of PTSD and MDD biomarkers to detect people at risk for the disorder since we linked the identified brain profiles with genetic risk. Excitingly, we have also associated our findings with brain imaging biomarkers that can be measured in patients to monitor disease status,” said senior author Nikolaos P. Daskalakis, MD, Ph.D., director of Neurogenomics and Translational Bioinformatics Laboratory at McLean Hospital.
“Our findings can also be used in the development of targeted treatments with cell type resolution. The observation of the neuronal glucocorticoid signaling pathway involvement means that neuron-specific glucocorticoid-based treatments could be developed compared with the current glucocorticoid treatments that affect most cell types, making them not specific and prone to side effects.”
Next steps that could bring this research closer to the clinic include studies involving stem cell–derived cells.
“Stem cell–derived cells exposed to stress agents could recapitulate brain stress pathology. Additional research could involve genetic and pharmacologic manipulations of these cells to study mechanisms and develop therapies,” said co-author Kerry J. Ressler, MD, Ph.D., chief scientific officer and chief of the Division of Depression and Anxiety Disorders at McLean Hospital.
“This study is very important because it provides a glimpse into how the brains of individuals struggling with PTSD and depression are similar and different at the cellular and molecular level in a critical region of the brain called the dorsolateral prefrontal cortex,” said Ned H. Kalin, MD, editor-in-chief, American Journal of Psychiatry.
“Using cutting-edge technology, the investigators established specific types of brain cells and specific genes within these cells that differ in their activity levels in relation to these stress-related and frequently co-occurring illnesses. The findings point the way to new cellular and drug targets that may benefit individuals with these disorders.”
More information:
Chris Chatzinakos et al, Single-Nucleus Transcriptome Profiling of Dorsolateral Prefrontal Cortex: Mechanistic Roles for Neuronal Gene Expression, Including the 17q21.31 Locus, in PTSD Stress Response, American Journal of Psychiatry (2023). DOI: 10.1176/appi.ajp.20220478
Journal information:
American Journal of Psychiatry
Source: Read Full Article
