Focal cortical dysplasia is a malformation of the cerebral cortex associated with one of the most severe types of epilepsy. Treatment is difficult owing to a lack of effective drugs or access to surgery. A new human model developed by researchers at the University of Campinas (UNICAMP) in the state of São Paulo, Brazil, using organoids cultured from patients’ cells has now opened up opportunities to test more specific therapies and medications.
In partnership with a group at the University of California San Diego (UCSD) in the United States, the researchers for the first time created cortical organoids that mimic focal cortical dysplasia and identified mechanisms that may be involved in the emergence of the anomaly during brain formation. They also obtained electrical readouts resembling the neuronal discharge typical of epileptic seizures in humans.
The results are reported in a paper in Brain, a leading clinical neurology and translational neuroscience journal. They can be the basis for future research to test drugs for patients with severe epilepsy, who continue to have frequent seizures after surgery or after taking prescription drugs for two years.
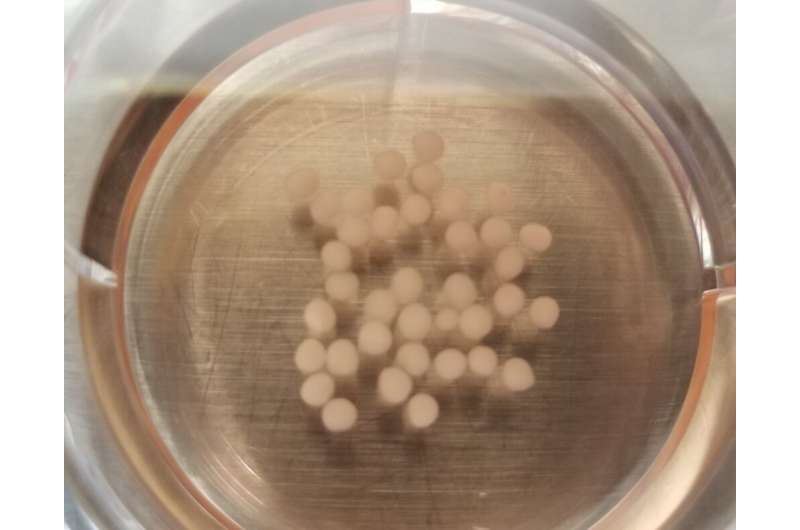
The organoids were cultured in vitro to simulate the morphology and functioning of part of the brain from skin cells donated by four patients with severe epilepsy treated at UNICAMP’s teaching hospital (Hospital de Clínicas). The cells were reprogrammed to become pluripotent stem cells and differentiate into neural cells.
Morphological, molecular and functional analysis of the organoids pointed to characteristics of this cortical malformation such as impaired cell proliferation, neuronal network hyperexcitability, dysmorphic neurons, and the presence of balloon cells, so called because of their shape, with a neuron-like nucleus and cytoplasm similar to an astrocyte’s.
“We observed molecular alterations compatible with what was expected in cellular pathways associated with neuron development and maturation. We also showed that it’s possible to create a cortical organoid with electrical activity resembling the neuronal discharges seen in epilepsy. In sum, our model mimics what we see in patients and can be used in future to screen existing medications,” Iscia Lopes-Cendes, a professor at UNICAMP’s Medical School and penultimate author of the paper, told Agência FAPESP.
Animal models are of limited usefulness in studies of this type of epilepsy because the cerebral cortex in rodents, for example, is very different from the human cortex and does not have similar malformations. “In the area of epilepsy, this is a very important study. Various attempts have been made, with successes and failures, over a period of many years. The result is a major reward for Simoni’s perseverance, a key quality in research,” said Lopes-Cendes, BRAINN’s principal investigator.
Epilepsy is an incurable neurological disease affecting some 50 million people worldwide, according to the World Health Organization (WHO). About 2 million cases have been reported in Brazil.
Patients with severe epilepsy may have 40-50 seizures per day, losing consciousness and collapsing. Treatment involves a combination of drugs, which do not always work. Most medications inhibit the activity of neurons in a generalized manner, controlling seizures but with many side effects, such as drowsiness and memory problems. Surgical removal of part of the brain is indicated in about 40% of patients with refractory seizure disorders after taking medication for a year.
Uncontrolled seizures not only have a highly adverse effect on the patient’s quality of life but constitute a major risk of premature sudden death, which can be as much as three times the average for the overall population. In addition, about half of all adults with epilepsy have other disorders such as depression and anxiety.
“We succeeded in mimicking the development of the neocortex and some hallmarks of focal cortical dysplasia,” Avansini said. “The advantage of our method was that we used a human model that maintained the patient’s genetic background. With an organoid, it’s possible to study each stage of the malformation, which starts with development of the cortex, with repercussions for cell proliferation and differentiation.”
The literature is not clear as to how abnormal cortical development contributes to the creation of epileptic seizures in dysplastic cortical tissue. Earlier research by the group, resulting from Avansini’s doctorate and reported in a 2018 article, suggested that dysregulation of the expression of the gene NEUROG2, important to the differentiation of neurons and glial cells (astrocytes, oligodendrocytes and microglia), plays a key role in development of the disease.
Sample
The researchers used skin cells from four patients who had not responded to treatment with medication or surgery. One had undergone three surgical procedures, which resulted in less frequent seizures but did not achieve the expected result. The other three had had two operations and included a child who started having convulsions at 14 months and whose speech had been partly impaired.
“Our data points to a molecular disruption in neuroepithelial junction cells affecting how some neurons form the cortical plate, leading to neural network alterations that make these patients susceptible to epilepsy,” Alysson Muotri, a professor at UCSD and last author of the Brain paper, says in a video about the study.
To capture the electrical data, the scientists used two techniques, one of which was an innovation in this field of research and involved inserting specially designed electrodes into the organoid. They succeeded in working with three-to-five-month-old organoids, which are hard to grow because most organoids die quickly for lack of a vascular system.
“We’re motivated by challenges,” Avansini said. “A relative of mine had epilepsy and died as a result of a seizure. When you experience something like that, you know exactly how families of patients feel. That’s what makes me tick. Our group has achieved progress in several ways but much remains to be done, and the search continues.”
Next steps, she explained, include trying to understand more about how epilepsy develops, focusing on the proliferative region to investigate how the cells and circuit are formed, and verifying whether interventions are feasible in the system as part of novel therapies.
Avansini is currently a researcher in the Bioimaging Division of the Brazilian Bioscience National Laboratory (LNBio), a research institution that uses synchrotron light and is part of the Brazilian Center for Research in Energy and Materials (CNPEM), alongside three other laboratories: Sirius, the National Synchrotron Light Laboratory (LNLS); the National Biorenewables Laboratory (LNBr); and the National Nanotechnology Laboratory (LNNano).
Source: Read Full Article