A new study has increased the understanding of an increasingly common complication of advanced breast cancer. Using a novel approach, researchers have uncovered details of secondary breast cancer in the brain and spinal cord that may help with developing effective treatments for people whose disease progresses in this way.
The study revealed for the first time that breast cancer leptomeningeal metastasis (BCLM) cells spread early from the primary breast tumor and that they acquire features typically associated with lobular breast cancer, which develops in the glands that produce breast milk.
The innovative approach taken by the researchers also allowed them to implant BCLM cells from five patients into mice to establish models of the disease that other researchers can use. This progress should fuel more research in this area.
This study was led by scientists at The Institute of Cancer Research, London, and it was published in the journal Nature Communications.
BCLM has been prohibitively challenging to study
BCLM occurs when breast cancer cells spread to the leptomeninges—the two layers of tissue lining the brain and spinal cord. It is estimated to affect 1 in 20 people with metastatic breast cancer, and there is currently no effective treatment.
This complication is becoming more common in metastatic cancer because the therapies that have been successful in prolonging life often do not control the disease in the brain or leptomeninges. However, relatively little has been known about the genetics or biology of this metastatic site until now.
This is primarily due to how rarely the site is biopsied. The short average survival following diagnosis leaves little time for a biopsy, and the procedure is complex. The leptomeninges cannot be accessed without creating an opening in the skull, and the structure of the metastases—which grow in a thin layer along the tissue rather than forming a single mass—makes it hard to obtain enough tumor material for analysis.
Innovative approach reaps rewards
For this study, researchers at the Breast Cancer Now Toby Robins Research Center at the ICR tried a different and less invasive way of obtaining material to analyze: liquid biopsies. Tumor cells release DNA, known as circulating tumor DNA (ctDNA), into bodily fluids, such as blood, where it contributes to cell-free DNA (cfDNA), a collection of DNA fragments released by various cells in the body. Collecting samples of these bodily fluids can reveal information about the cancer and its interactions with its environment.
Previous studies have used DNA sequencing technology, called next-generation sequencing, to detect variants and mutations in a limited number of genes in the cerebrospinal fluid (CSF). However, this study was the first to perform large-scale (whole exome) next-generation sequencing covering all 20,000 genes in both plasma, the liquid component of blood, and CSF from the same patient.
In addition, tissues from the original breast cancer tumor and from other sites to where the cancer had spread were sequenced. This approach made it possible to compare the genetic material of leptomeningeal metastasis cells with that of other sites in the body.
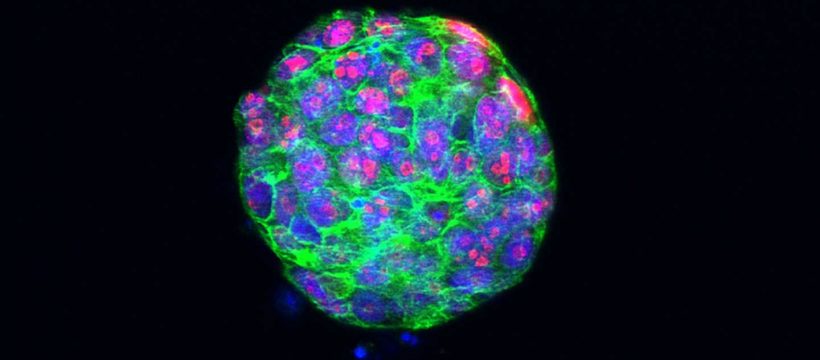
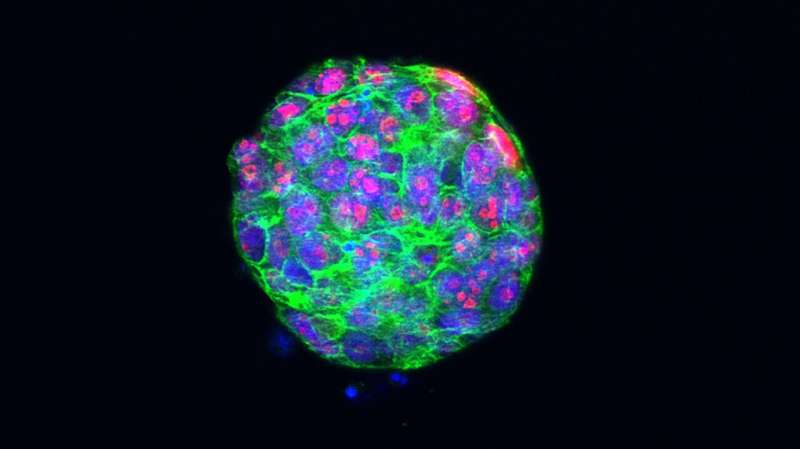
In addition, the team used disseminated tumor cells (DTCs)—malignant cells that had detached from the primary tumor and spread to the leptomeninges—to create 3D culture models. These mini-tumors, which simulate a physiological environment where the cells can interact with their surroundings, helped the researchers understand BCLM in more detail.
Learning more about BCLM
Comparisons between the samples revealed that the leptomeningeal metastasis cells had acquired additional mutations, including some that could affect the response to treatment. As a result, the BCLM genetic material was clearly distinct from that of the primary breast tumor. Of the total number of mutations present in CSF cfDNA and the primary tumor, 48% were only in CSF cfDNA while 20% were only in the primary tumor. Similarly, of all the mutations in the CSF cfDNA and the plasma cfDNA, 25% were only in the former while 17% were only in the latter.
By using a visual analysis tool called ClonEvol to look at the evolution of BCLM, the team also confirmed that BCLM starts to differ genetically from the primary tumor at an early stage. Together, these findings suggest that BCLM evolves in such a way as to enhance its survival within the leptomeningeal site.
Based on their observations of the DTCs, the authors state that this biological adaptation also gives the cells a growth advantage in endocrine organs, which include the ovaries. They believe that this is indicative of the cells becoming similar to lobular breast cancer cells, which use hormones—present in endocrine organs—to grow. This theory was supported by the higher loss of E-cadherin expression in CSF cfDNA samples than in primary tumor and plasma cfDNA samples. A low expression of the E-cadherin protein is associated with lobular breast tumors.
Finally, comparing leptomeningeal metastases with metastases elsewhere in the body revealed further evolutionary differences, with plasma cfDNA having been more affected than CSF cfDNA by chemotherapy. This suggests that the blood-brain and blood-CSF barriers shield cancer cells in the leptomeninges to some extent.
Creating future research opportunities
This work showed that it is possible to use CSF cfDNA and DTCs to investigate BCLM, meaning that the challenge of conducting a biopsy of the leptomeningeal site need not pose a barrier to other researchers. The wider research community can also benefit from the patient-derived models that the researchers created, which give them access to the cells they need to study in a setting that closely mimics the real one.
First author Dr. Amanda Fitzpatrick is already planning the next stage of her research, in which she will look more closely at BCLM genetics.
Dr. Fitzpatrick, an oncologist and honorary senior lecturer who has recently moved from the Molecular Cell Biology Group at the ICR to the Comprehensive Cancer Center at King’s College London, said, “We now know that certain genetic alterations are more common in leptomeningeal metastasis than in other types of breast cancer spread. These alternations involve genes that control cell shape and how cells stick to each other. The next steps are to understand how these changes provide cells with a growth advantage in the leptomeningeal space and to perform genetic perturbation screens to identify novel therapies.”
The current therapy used in leptomeningeal metastasis is invasive, involving the intrathecal delivery of methotrexate via lumbar puncture, and not very effective. The next stage of this research aims to identify novel drug treatments, ideally those that penetrate the blood-brain and blood-CSF barriers. These could be delivered in the form of a tablet or IV infusion, so they would also be less invasive.
Lead author Professor Clare Isacke, Professor of Cell Molecular Biology and Dean of Academic and Research Affairs at the ICR, said, “This work has achieved significant insights into breast cancer metastasis to the leptomeninges, which has been relatively unstudied to date. It is essential that we find new therapies that can control the cancer in this site so that people with advanced breast cancer can live longer with the disease. In our cohort, for example, two thirds of the patients had stable or absent breast cancer in the rest of their body but active cancer growth in the leptomeninges.
“We hope that our models and discoveries serve as valuable resources for other researchers in this area. In time, with more lab research, we are optimistic that we will be able to discover better treatments for people with this type of breast cancer spread.”
Dr. Kotryna Temcinaite, Head of Research Communications at Breast Cancer Now, said, “With 11,500 women dying from breast cancer in the U.K. every year, it’s vital we continue to fund research to better understand and treat this disease … this innovative research has brought us new understanding of how breast cancer that has spread to the lining of the brain and spinal cord differs from tumors in the breast and in other parts in the body, developing better ways to study the disease in the lab and test new treatments. We hope it will lead to better outcomes for people diagnosed with this devastating form of breast cancer in the future.”
More information:
Amanda Fitzpatrick et al, Genomic profiling and pre-clinical modelling of breast cancer leptomeningeal metastasis reveals acquisition of a lobular-like phenotype, Nature Communications (2023). DOI: 10.1038/s41467-023-43242-x
Journal information:
Nature Communications
Source: Read Full Article