For the first time, researchers performed a successful in-utero surgery to repair a potentially deadly developmental condition by treating an aggressive vascular malformation, called vein of Galen malformation, in a fetus's brain before birth, according to new research published today in Stroke, the peer-reviewed flagship journal of the American Stroke Association, a division of the American Heart Association.
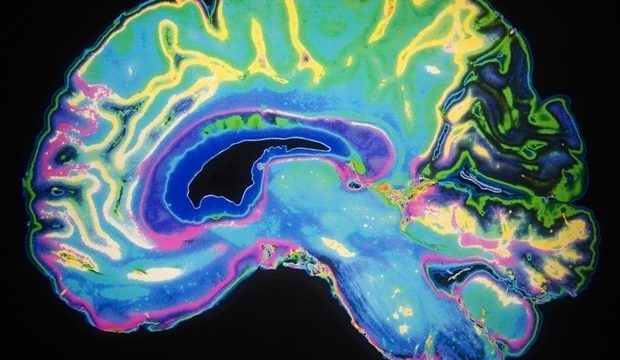
Vein of Galen malformation (VOGM) is a rare prenatal condition in which arteries bringing high-flow, high-pressure blood to the brain from the heart connect directly with one of the main collecting veins deep at the base of the brain, rather than to capillaries that are necessary to slow blood flow and deliver oxygen to surrounding brain tissue. Due to changes in the infant's vascular physiology during and after the birth process, the high flow in the malformation has an even more serious effect on the heart and brain after birth, putting enormous pressure on the newborn's heart and lungs. This may lead to pulmonary hypertension, heart failure or other potentially life-threatening conditions. VOGM is most often first seen on a prenatal ultrasound and is definitively diagnosed by MRI during the late second or third trimester of pregnancy.
The researchers performed the in-utero embolization on a fetus with VOGM at 34 weeks and 2 days gestational age, as the first treated patient in a clinical trial that is underway at Boston Children's Hospital and Brigham and Women's Hospital, performed with oversight from the U.S. Food and Drug Administration.
In our ongoing clinical trial, we are using ultrasound-guided transuterine embolization to address the vein of Galen malformation before birth, and in our first treated case, we were thrilled to see that the aggressive decline usually seen after birth simply did not appear. We are pleased to report that at six weeks, the infant is progressing remarkably well, on no medications, eating normally, gaining weight and is back home. There are no signs of any negative effects on the brain."
Darren B. Orbach, M.D., Ph.D., lead study author, co-director of the Cerebrovascular Surgery & Interventions Center at Boston Children's Hospital and an associate professor of radiology at Harvard Medical School
Due to premature rupture of membranes during the in-utero embolization, the infant was delivered by induction of vaginal birth two days later. Echocardiography after birth showed progressive normalization of cardiac output. In this case, the newborn did not require any cardiovascular support or surgery following the in-utero treatment and was watched in the NICU for several weeks after birth because of prematurity before being sent home. During that time, the newborn had a normal neurological exam and showed no strokes, fluid buildup or hemorrhage on brain MRI.
"While this is only our first treated patient and it is vital that we continue the trial to assess the safety and efficacy in other patients, this approach has the potential to mark a paradigm shift in managing vein of Galen malformation where we repair the malformation prior to birth and head off the heart failure before it occurs, rather than trying to reverse it after birth," Orbach said. "This may markedly reduce the risk of long-term brain damage, disability or death among these infants."
It is estimated that VOGM, the most common congenital vascular brain malformation, occurs in as many as one in every 60,000 births. The current standard of care for VOGM is treatment after birth with embolization, a catheter-based procedure to close off the direct artery-to-vein connections in the malformation and block the excess blood flow to the brain and heart. However, embolization itself is high risk and is not always successful at reversing heart failure. Additionally, severe brain damage may have already occurred, which may lead to life-long cognitive disabilities and life-threatening conditions for the infant, or even to death.
"The fetal intervention team at Boston Children's Hospital and Brigham and Women's Hospital have successfully devised another in utero procedure that may be very impactful in a specific group of patients diagnosed with vein of Galen malformation," said Gary M. Satou, M.D., FAHA, the director of pediatric echocardiography at UCLA Mattel Children's Hospital and co-director of the UCLA Fetal Cardiology Program and who was not involved with the study. Satou, a pediatric cardiologist, is past chair of the American Heart Association's Congenital Cardiac Defects committee of Young Hearts Council and a clinical professor in the department of pediatrics at the David Geffen School of Medicine at UCLA.
"As always, a number of these fetal cases will need to be performed and followed in order to establish a clear pattern of improvement in both neurologic and cardiovascular outcomes," Satou said. "Thus, the national clinical trial will be crucial in order to achieve adequate data and, hopefully, successful outcomes."
The procedure was not without its limitations, noted Colin P. Derdeyn, M.D., a neurointerventional radiologist at University of Iowa Health Care who performs VOGM embolizations on neonates and who was not involved with the study.
"The key advance here is to intervene before the physiologic events of birth can cause life-threatening heart failure. There are caveats; one successful case is not enough experience for us to conclude that the risks of this procedure are worth the benefits. Safety issues may crop up in future procedures, and this approach through the veins may not be consistently successful in preventing heart failure. The procedure described here is designed to reduce the flow through the malformation and not to cure it," said Derdeyn, the Krabbenhoft Professor of Radiology and chair and department executive officer of the department of radiology at the University of Iowa Health Care Carver College of Medicine and a past chair of the American Heart Association's Stroke Council.
"However, the positive hemodynamic changes that they observed in utero and after birth – reduction in flow, reduction in size of the draining vein, reversal of the abnormal reversed flow in the aorta – are really encouraging. These are some of the most exciting and surprising aspects of this case report," he said. "This is pioneering work being done in a very careful and responsible way."
Co-authors are Louise E. Wilkins-Haug, M.D.; Carol B. Benson, M.D.; Wayne Tworetzky, M.B. Ch.B.; Shivani D. Rangwala, M.D.; Stephanie H. Guseh, M.D.; Nicole K. Gately, R.N.; Jeffrey N. Stout, Ph.D.; Arielle Mizrahi-Arnaud, M.D.; and Alfred P. See, M.D. Authors' disclosures are listed in the manuscript.
The study was funded by a grant from the Sage Schermerhorn Chair for Image-Guided Therapy (DBO) in Boston Children's Hospital's Radiology Department.
American Heart Association
Orbach, D. B., et al. (2023). Transuterine Ultrasound-Guided Fetal Embolization of Vein of Galen Malformation, Eliminating Postnatal Pathophysiology. Stroke. doi.org/10.1161/strokeaha.123.043421.
Posted in: Child Health News | Medical Procedure News | Medical Research News
Tags: Aorta, Blood, Brain, Capillaries, Cardiology, Catheter, Children, Clinical Trial, CT, Disability, Efficacy, Food, Health Care, Health Insurance, Heart, Heart Failure, Hospital, In Utero, Lungs, Medical School, Medicine, Newborn, Oxygen, Pathophysiology, Pediatrics, pH, Physiology, Pregnancy, Prenatal, Pulmonary Hypertension, Radiology, Research, Stroke, Surgery, Ultrasound, Vaginal, Vascular
Source: Read Full Article