An international study led by researchers from the Infection Biology Laboratory at the UPF Department of Medicine and Life Sciences (MELIS) establishes that one type of dendritic cell is crucial for the success of immunotherapeutic treatments to control chronic viral infections. These dendritic cells have been found to be key in reactivating exhausted lymphocytes responsible for clearing infected cells to keep the viral load low.
Chronic viral infections, such as those caused by human immunodeficiency virus (HIV) or hepatitis B and C viruses, are characterized by a persistent viral load. This is maintained by a balance between the expansion of the virus and the expansion of exhausted T lymphocytes, which—once the viral load increases—become active, multiply and eliminate infected cells.
In HIV-infected patients, infection has been controlled with antiviral therapy that reduces the viral load to below detectable levels. However, this is transitory, as the viral load increases dramatically when treatment is stopped. With 650,000 people worldwide dying from HIV and 1.5 million acquiring the virus each year, there is a need to find a functional cure that controls the virus without causing disease and avoids the side effects and burden on health systems that antiviral therapy entails.
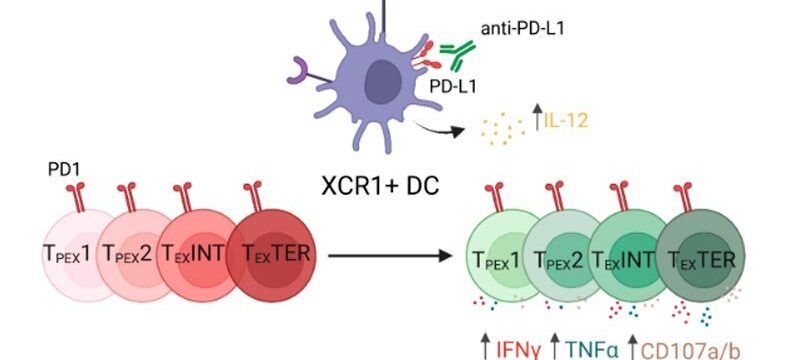
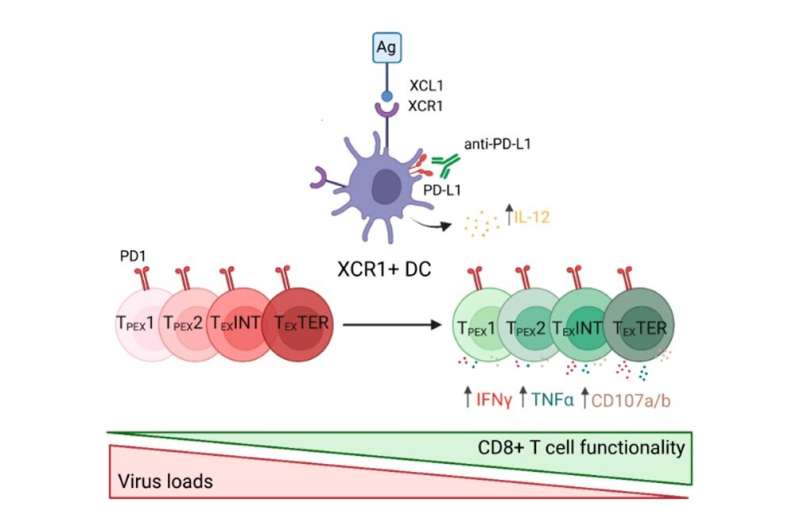
Hence, immunotherapies based on checkpoint inhibitors that block proteins preventing the immune system from attacking infected cells are considered a promising therapy.
The study published in Cell Reports determines that the various types of dendritic cells differ in their ability to reactivate exhausted lymphocytes during checkpoint immunotherapy. It also identifies XCR1+ cross-presenting dendritic cells as key elements that trigger exhausted lymphocyte reactivation in checkpoint inhibitor-based immunotherapies. Therefore, XCR1+ cross-presenting dendritic cells are a promising therapeutic target to improve virus control during chronic viral infection.
The study, performed in a mouse model of the chronic lymphocytic choriomeningitis virus—which partly resembles human chronic HIV and hepatitis virus infections—opens the possibility of considering combination immunotherapies including checkpoint inhibitors that target cross-presenting dendritic cells as an interesting therapy option for HIV-infected individuals.
“Our findings are an important step forward in understanding the requirements for cure strategies in chronic infections,” says Eva Domenjo, first author of the manuscript. “The next steps now are to improve the duration of the therapeutic benefits and translate the data from the model system to the clinical practice,” adds Andreas Meyerhans, who coordinated the work together with Jordi Argilaguet.
Considering analogous findings in cancer immunotherapy, this not only argues for immunological similarities between chronic infections and cancers, but also gives hope for a timely translation into clinical applications.
More information:
Eva Domenjo-Vila et al, XCR1+ DCs are critical for T cell-mediated immunotherapy of chronic viral infections, Cell Reports (2023). DOI: 10.1016/j.celrep.2023.112123
Journal information:
Cell Reports
Source: Read Full Article