Researchers in the United States have conducted a study suggesting that the coronavirus disease 2019 (COVID-19) vaccines that are currently being rolled out in many countries should be effective against the C.37 lineage (lambda variant) of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The C.37 lineage, which has been categorized as a “variant of interest” by the World Health Organization, is currently increasing in prevalence in South American and other countries.
The researchers found that while pseudotyped virus expressing the C.37 viral spike protein was less susceptible to vaccine-elicited neutralizing antibodies, the reduction in neutralization was only minor.
The spike protein is the main surface structure that SARS-CoV-2 uses to bind to and infect host cells. The receptor-binding domain (RBD) of this spike mediates the initial stage of the infection process when it binds to the host cell receptor angiotensin-converting enzyme 2 (ACE2).
The team – from the New York University Grossman School of Medicine – says the study findings also suggest that Regeneron’s REGN-COV2 cocktail of monoclonal antibodies should be effective against C.37.
“The results suggest that the vaccines in current use will remain protective against the lambda variant and that monoclonal antibody therapy will remain effective,” writes Nathaniel Landau and colleagues.
A pre-print version of the research paper is available on the bioRxiv* server, while the article undergoes peer review.
.jpg)
Concerns surrounding continued emergence of SARS-CoV-2 variants
The ongoing emergence of SARS-CoV-2 variants containing mutations that confer increased transmissibility or immune escape are increasingly causing concern about the immunity provided by previous infection or vaccination.
“The spread of variants also raises concerns regarding a potential decrease in the efficacy of anti-spike protein monoclonal antibody therapies that have been shown to reduce disease symptoms and the rate of hospitalization,” says Landau and colleagues.
The C.37 spike protein is characterized by several novel deletions and mutations, two of which are found in the RBD.
“The lambda spike protein contains novel mutations within the RBD (L452Q and F490S) that may contribute to its increased transmissibility and could result in susceptibility to re-infection or a reduction in protection provided by current vaccines,” says the team.
What did the current study involve?
The researchers tested the infectivity and susceptibility of lentivirus pseudotyped with the C.37 spike protein to neutralization by convalescent sera, vaccine-elicited antibodies and the Regeneron monoclonal antibodies REGN10933 and REGN10987.
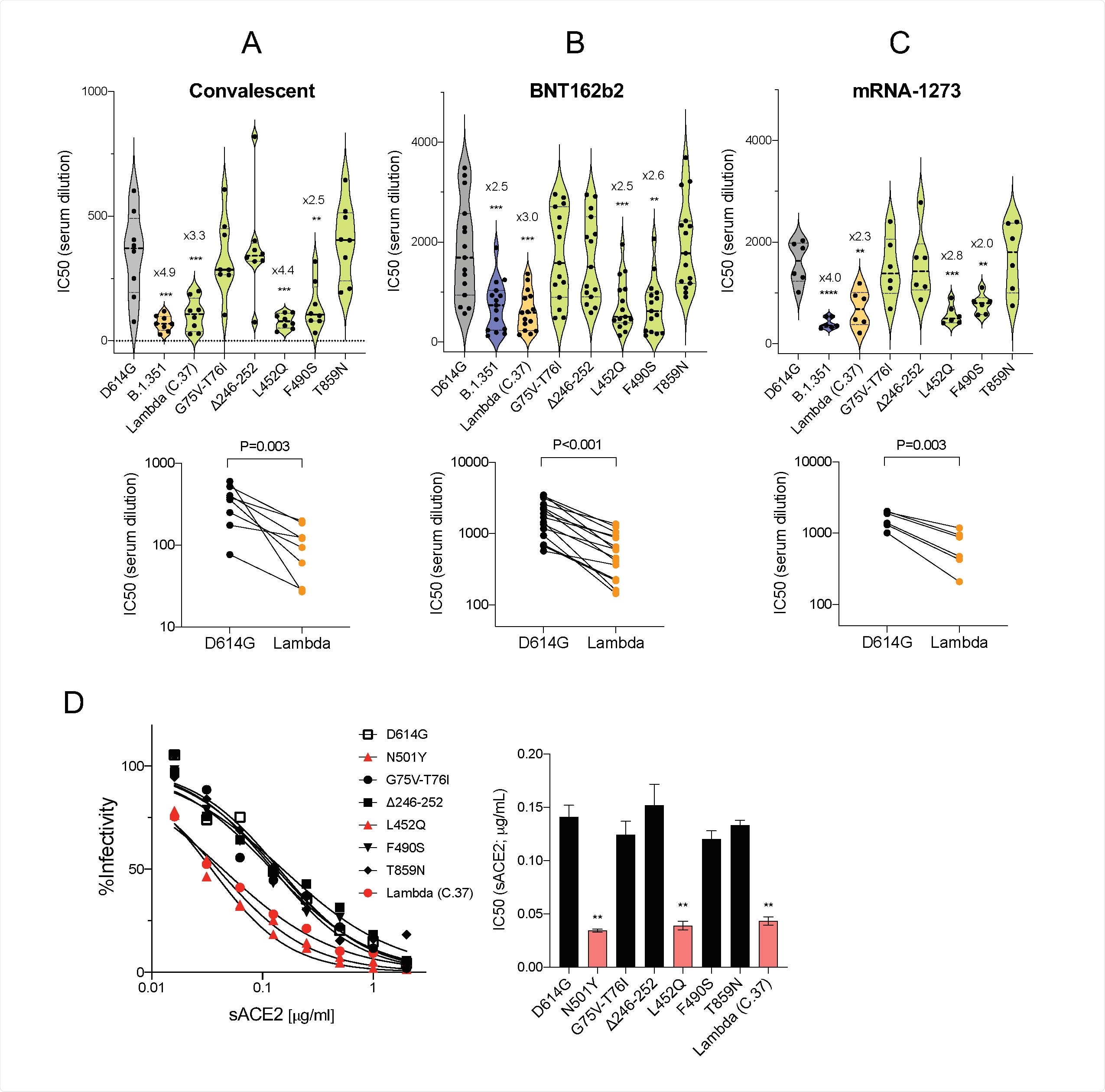
The C.37 spike virus exhibited a 2-fold increase in the infectivity of ACE2.293T cells, compared with the virus containing the D614G spike mutation that emerged and became dominant soon after the COVID-19 pandemic began.
Landau and colleagues report that this increased infectivity was attributed to the L452Q mutation. None of the other mutations (G75V-T76I, F490S, T859N and D246-252) significantly impacted infectivity.
Analysis of serum samples from convalescent patients who had been infected prior to the emergence of SARS-CoV-2 variants showed that the C.37 spike virus was 3.3 times more resistant to neutralization, compared with the D614G spike virus.
Similarly, analysis of serum from individuals who had been immunized with Pfizer-BioNTech’s BNT162b2 vaccine or Moderna’s mRNA-1273 vaccine showed that the C.37 spike virus was about 3.0 and 2.3 times more resistant, respectively, to neutralization.
The researchers report that the increased resistance to neutralization was attributed to the presence of the C.37 spike mutations L452Q and F490S.
What about the effectiveness of Regeneron’s monoclonal antibodies?
Next, the team tested the effectiveness of Regeneron’s monoclonal antibodies – REGN10933 and REGN10987 – on viruses expressing the C.37 spike or the D614G spike.
This revealed that the C.37 spike virus was approximately 3.6 times more resistant to neutralization by REGN10987 – an outcome that was attributed to the L452Q mutation.
However, the C.37 spike virus was effectively neutralized by Regeneron’s REGN-COV2 cocktail therapy containing both REGN10933 and REGN10987, with no decrease in neutralizing titers observed, compared with titers against the D614G spike virus.
What do the authors advise?
The team says that while the lambda spike protein showed partial resistance to neutralization by vaccine-elicited antibodies and convalescent sera, the average 3-fold decrease in neutralizing titer against the variant is not likely to result in any significant loss of protection against infection.
Furthermore, “while the lambda variant was slightly resistant to REGN10987, it was neutralized well by the cocktail with REGN10933,” they add.
However, Landau and colleagues warn that although the findings suggest that current vaccines will provide protection against the variants identified to date, the results do not preclude the possibility that novel variants will emerge that are more resistant to current vaccines.
“The findings highlight the importance of wide-spread adoption of vaccination which will protect individuals from disease, decrease virus spread and slow the emergence of novel variants,” they conclude.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Landau N, et al. SARS-CoV-2 Lambda Variant Remains Susceptible to Neutralization by mRNA Vaccine-elicited Antibodies and Convalescent Serum. bioRxiv, 2021. doi: https://doi.org/10.1101/2021.07.02.450959, https://www.biorxiv.org/content/10.1101/2021.07.02.450959v1
Posted in: Drug Trial News | Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antibody, Cell, Coronavirus, Coronavirus Disease COVID-19, Efficacy, Enzyme, immunity, Lentivirus, Medicine, Monoclonal Antibody, Mutation, Pandemic, Protein, Receptor, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Vaccine, Virus

Written by
Sally Robertson
Sally first developed an interest in medical communications when she took on the role of Journal Development Editor for BioMed Central (BMC), after having graduated with a degree in biomedical science from Greenwich University.
Source: Read Full Article
