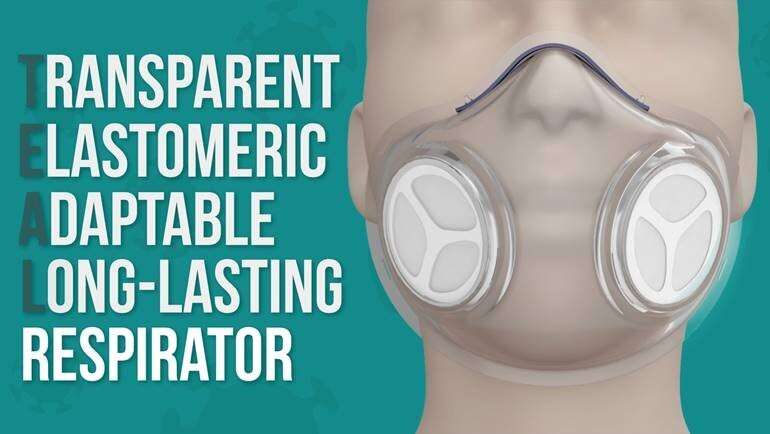
Investigators from Brigham and Women’s Hospital and Massachusetts Institute of Technology have been working to design a better, reusable respirator that could serve as an alternative to an N95 respirator. In the latest iteration of their work, they have introduced sensors to inform the user if the respirator is on properly and whether the filters are becoming saturated. The team tested the respirator, known as the transparent, elastomeric, adaptable, long-lasting (TEAL) respirator, at the Brigham and at Massachusetts General Hospital (MGH), and reports a 100 percent success rate for fit testing among 40 participants, with feedback demonstrating exceptional fit, breathability and filter exchange. Results are published in ACS Pharmacology & Translational Science.
“During the COVID-19 pandemic, the need for respirators and masks has been urgent. Our team has worked to develop a respirator platform that not only fits comfortably and snugly but can also be sterilized and re-sterilized,” said corresponding author Giovanni Traverso, MB, BChir, Ph.D., a gastroenterologist and biomedical engineer in the Division of Gastroenterology at the Brigham and assistant professor in the Department of Mechanical Engineering at MIT. “In this study, we looked at up to 100 re-sterilization cycles and found that the TEAL respirator we’ve designed can withstand that.”
The team evaluated 7 different methods for repeatedly sterilizing the TEAL respirator, including 100 cycles of autoclaving, 100 cycles of microwaving, prolonged exposure to UV treatment, high heat (200 °C), 100 percent isopropyl alcohol, and bleach. The researchers found minimal change to the respirator’s elasticity after repeated sterilization.
The TEAL respirator is comprised of a transparent, stretchy shell that can be sterilized and filters that can be replaced by the user. The team found that all participants could successfully replace their filters and most participants (90 percent) reported an excellent or good fit for the respirator.

“TEAL is the first elastomeric respirator designed for use in a surgical setting, preserving the sterile field and providing the user a comfortable, reusable personal protective equipment solution,” said co-author Adam Wentworth, MS, a senior research engineer in the Brigham’s Division of Gastroenterology and the Traverso lab.
The respirator’s sensors can help detect respiratory rate, exhalation temperature, and exhalation and inhalation pressures. The team also added a thermochromic coating to the respirator—a coating that changes color from black to pink when the respirator is in direct contact with a person’s face and therefore has a snug fit.
The researchers evaluated the respirator’s performance in a clinical setting, enrolling 47 subjects from the Brigham and MGH (40 of the subjects underwent fit testing). Participants were asked to score the respirator on its fit, breathability and ease of filter exchange, and were also asked if they preferred the TEAL respirator to other options. Of those queried, 60 percent preferred the TEAL respirator compared to 5 percent who preferred standard hospital-supplied respirators. The remaining 35 percent had no preference.
“We were excited to receive the feedback from the trial participants that they would love to continue using and testing the respirator, given its comfort, transparency and ease of use,” said co-author James Byrne, MD, Ph.D., a resident in the Department of Radiation Oncology at the Brigham and a postdoctoral fellow in the Traverso lab.

Byrne notes that in addition to its other features, the TEAL respirator’s transparency may offer some advantages over more traditional respirators.
“One of the big benefits of the TEAL respirator is that it enables visualization of the lips,” he said. “This can be immensely helpful in communication and expression, especially during this time when communication through N95 respirators and surgical masks makes it challenging to understand one another.”
The sample size of the study was small, and the investigators acknowledge the importance of additional evaluation in a larger cohort of individuals and over a longer timeframe to further test the respirator’s functionality. To use the respirator in a health care setting, additional testing according to National Institute for Occupational Safety and Health (NIOSH) criteria will be needed.
Source: Read Full Article
