Previous research has suggested that the severe acute respiratory syndrome 2 (SARS-CoV-2) virus affects the brain and causes enduring neurological problems. However, how the virus causes various neurological complications and long-term mental health problems remains under investigation.
A new study by researchers in Croatia and Slovenia shows the SARS-CoV-2 spike protein has an affinity towards monoamine oxidases (MAO) enzymes. Changes in MAO levels have been the culprit for several neuropsychiatric disorders such as Parkinson’s or Alzheimer’s disease.
The researchers write:
“…Our work aids in identifying the critical role of the MAO enzymes towards an increased incidence of neurological disorders in the SARS‐CoV‐2 infected individuals, therefore placing a neurobiological link between these two conditions in the spotlight.”
A SARS-CoV-2–MAO complex formation significantly reduced brain MAO activity by lowering MAO affinity toward neurotransmitters. Based on the findings, the researchers suggest the complex could increase the risk of developing a neurodegenerative illness in people infected with COVID-19.
The study “Relationship between COVID-19 infection and neurodegeneration: Computational insight into interactions between the SARS-CoV-2 spike protein and the monoamine oxidase enzymes” is available on the bioRxiv* preprint server while awaiting peer review.
.jpg)
Validating computational protocol and SARS-CoV-2 binding affinity
The research team created a computer model to evaluate spike protein-ACE2 binding and docking features. Then, they narrowed their focus to the Beta variant with a high ACE2 binding affinity and increased infectivity.
A decomposition of the binding affinity revealed several spike protein residues playing a major role in ACE2 binding.
About 15 spike protein residues belonged to the receptor-binding motif of the receptor-binding domain. They comprised 78% of the total binding energy. The only exception was Lys417 which instead forms a salt bridge with Asp30 from ACE2.
The most dominant residue is Tyr501, a mutation of Asn501 in the original SARS-CoV-2 strain. This residue makes up 17% of binding energy. Additionally, the N501Y mutation in the Beta variant helps to increase the residue’s binding affinity.
Spike protein residues that do not favor binding include Asp405 and Glu406. These residues are not located in the receptor-binding motif of the receptor-binding domain.
The results confirm the original SARS-CoV-2 strain and Beta variant are similar in recognizing ACE2. It also showed that the order of residues contributing to binding remains unchanged, suggesting the spike protein mutations in the Beta variant are responsible for approximately 70% of the overall binding affinity.
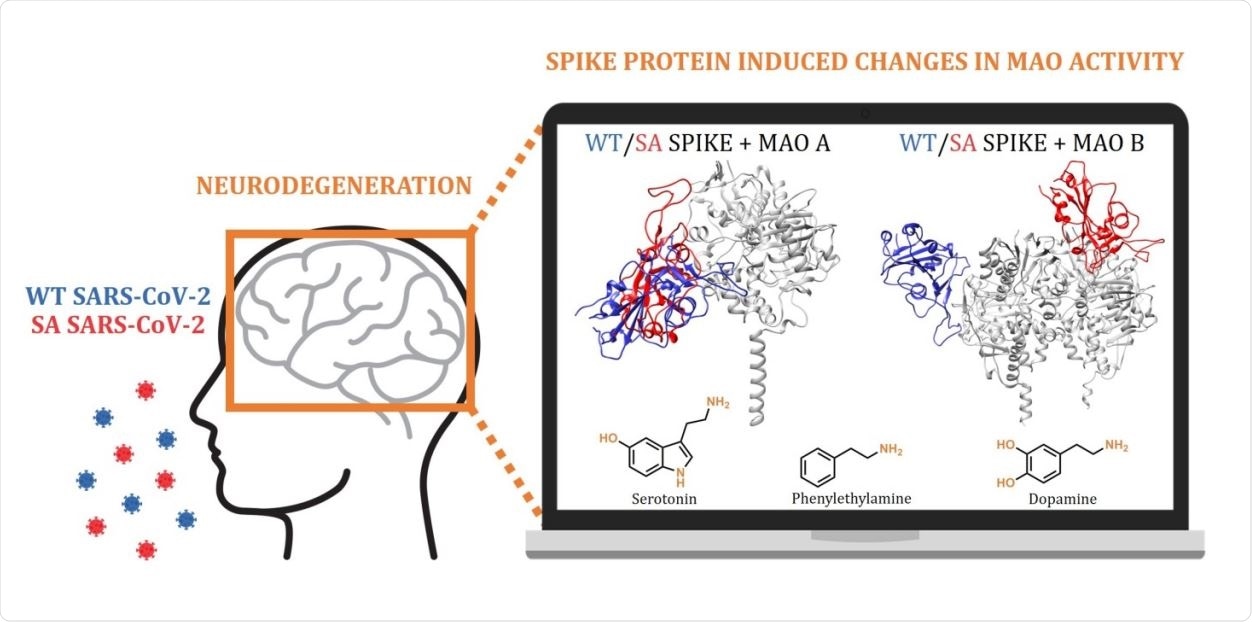
MAO-A and MAO-B enzymes interact with Beta variant
The researchers used the validating computation set up to investigate potential interactions between the SARS-CoV-2 strains and MAO enzymes. Results showed SARS-CoV-2 links with MAO enzymes through spike protein residues in the receptor-binding motif residue. In addition, the binding affinity towards MAO enzymes increases in more infectious variants.
In the Beta variant, all three of its spike protein mutations promote MAO-A binding. The mutated Asn417 residue appears to contribute the most to the binding of MAO-A, which could indicate the formation of a SARS-CoV-2 beta variant–MAO-A complex.
Two spike protein residues in the Beta variant, S-Leu455 and the mutated Asn417, use their backbone carbonyl and side-chain amide atoms to engage with MAO A’s Arg297 residue.
The Beta variant has a higher binding affinity with MAO B than with the ACE2 receptor. A possible reason for the high affinity is the location of different MAO B areas subunits. The researchers suggest the favorable binding between the two could influence the progression of neurological conditions.
High binding affinity towards MAO negatively impacts MAO interactions with brain amines
The affinity between MAO isoforms and the original SARS-CoV-2 strain affects its interaction with phenylethylamine, serotonin, and dopamine.
The virus’s impact on MAO’s binding to other substrates is affected even further with the Beta variant. The Beta variant increases MAO affinity towards its substrates and induces higher rates of metabolic degradation, resulting in their depletion.
“Since the obtained insight suggests that a more contagious SA variant causes even larger disturbances, and with new and more problematic strains likely emerging in the near future, we firmly advise that the presented prospect of the SARS-CoV-2 induced neurological complications should not be ignored, but rather requires further clinical investigations to achieve an early diagnosis and timely therapeutic interventions,” conclude the team.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Hok L, et al. Relationship between COVID-19 infection and neurodegeneration: Computational insight into interactions between the SARS-CoV-2 spike protein and the monoamine oxidase enzymes. bioRxiv, 2021. doi: https://doi.org/10.1101/2021.08.30.458208, https://www.biorxiv.org/content/10.1101/2021.08.30.458208v1
Posted in: Medical Research News | Medical Condition News | Disease/Infection News
Tags: ACE2, AIDS, binding affinity, Brain, Coronavirus Disease COVID-19, Dopamine, Mental Health, Mutation, Neurodegeneration, Protein, Receptor, Research, Respiratory, SARS, SARS-CoV-2, Serotonin, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Virus

Written by
Jocelyn Solis-Moreira
Jocelyn Solis-Moreira graduated with a Bachelor's in Integrative Neuroscience, where she then pursued graduate research looking at the long-term effects of adolescent binge drinking on the brain's neurochemistry in adulthood.
Source: Read Full Article
