High-density lipoprotein (HDL) cholesterol, often called “good cholesterol,” removes extra cholesterol from the arteries by gobbling up early-forming plaque and transporting it to the liver, which flushes it out of the body. It’s an essential job: when too much plaque accumulates in the arteries, it can narrow blood vessels and impede blood flow, or even rupture. This can lead to severe events, including heart attacks and stroke.
Measuring how much HDL cholesterol we have in our bodies to do these tasks has long been a mainstay of the annual physical. However, within the past decade, researchers have also found that measuring whether HDL cholesterol is doing these tasks effectively can be just as valuable. The stronger the signs that a person’s “good cholesterol” is working well, they’ve discovered, the more likely they appear to have reduced risks for heart disease in the future.
There’s been one main challenge, however. Measuring HDL function is limited to research labs and isn’t conducive to large-scale testing by routine clinical laboratories. To try to solve that problem, researchers from NHLBI’s Lipoprotein Metabolism Laboratory created a new diagnostic test.
“This is going to quicken the pace of basic research,” said Edward B. Neufeld, Ph.D., a scientist in the lab who, along with Masaki Sato, Ph.D., developed the test. “It increases the number of samples that you can study. It increases the number of experiments you can do.”
Current HDL functional assessments require researchers to harvest cells in the lab. This has to be done in small batches, often requires extra materials like radioactive cholesterol, and can take days to process. The cell-free test that Neufeld and researchers developed could be easily replicated in labs, automated to process larger samples, and provide readings in about an hour. Importantly, they have shown in clinical studies that their test can predict cardiovascular disease risk better than HDL cholesterol, which is currently used to assess such risk. They published these findings in the Journal of Clinical Investigation.
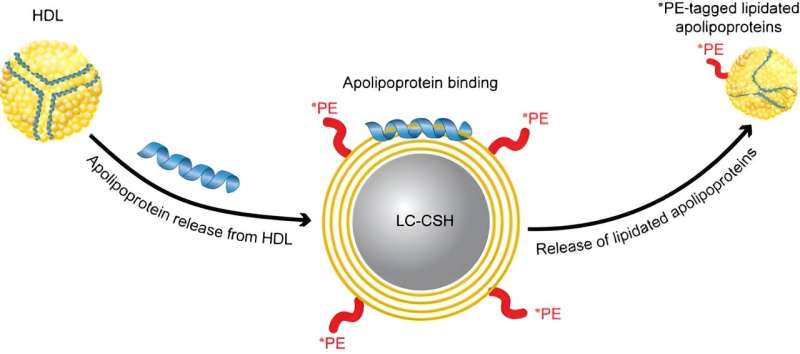
To perform the test, a person’s plasma, which contains HDL, is separated from their blood. The plasma is added to donor particles coated with a lipid mixture that resembles plaque, and a fluorescent-tagged phospholipid that can only be removed by HDL. The fluorescent signal obtained by HDL is then measured. A brighter signal reflects optimal HDL lipid removal function. A dim light indicates reduced function.
The test is still years away from potential use in a medical setting, but it holds promise for physicians looking to gather additional information that could help inform their treatment decisions.
For example, a patient with intermediate risk for having a heart attack or stroke in 10 years, also found to have reduced HDL function, may emerge as a stronger candidate for treatment or for having additional assessments to measure how much atherosclerotic plaque they have. “Any additional information that we could get in terms of assigning stratification would be of great benefit,” said Neufeld. He explained that many adults have medium-level risks.
NIH has now patented the test and will work with an outside company to purchase the rights to license and manufacture the diagnostic material. “Other people may modify this or come up with better versions, which is fine with us,” said Neufeld. “We just really wanted to tackle this problem of evaluating HDL function.”
Neufeld and his colleagues believe the test could also be used for multiple purposes in research, which could lead to clinical applications, such as use in the doctor’s office. This excites them, but they caution that they still have a lot to learn. “HDL cholesterol is important, but we still don’t fully understand it,” said Alan T. Remaley, M.D., Ph.D., a senior investigator in the Lipoprotein Metabolism Laboratory. “Biology is full of mysteries.”
Remaley explained that while HDL cholesterol research has transformed cardiovascular research, therapeutic advancements to improve HDL cholesterol haven’t followed. “Someday we may have a drug that modulates HDL and turns out to be beneficial, but right now we don’t have that,” said Remaley.
“There’s a long tradition in the field of knowing that research takes time,” Remaley explained. Like for other disciplines, incremental advancements in lipoprotein research have led to novel discoveries.
He and Neufeld envision that the updated HDL function test, which builds on previous findings, will support similar advancements. “This could open up new opportunities to gain further insights, such as with drug development, that have been difficult to achieve,” said Neufeld.
More information:
Masaki Sato et al, Cell-free, high-density lipoprotein–specific phospholipid efflux assay predicts incident cardiovascular disease, Journal of Clinical Investigation (2023). DOI: 10.1172/JCI165370
Journal information:
Journal of Clinical Investigation
Source: Read Full Article
